3 interesting studies on COVID-19
It's been more than a year since the outbreak of COVID-19.
The corona pandemic situation shows no signs of ending at any time.
Researchers around the world are conducting numerous studies to understand the characteristics of this virus and its mechanisms for the development of vaccines and treatments. Major countries around the world are making all-out efforts to prevent the spread of COVID-19 and develop treatments, and we would like to introduce some interesting research results related to COVID-19.
1. Can I get COVID from sex?
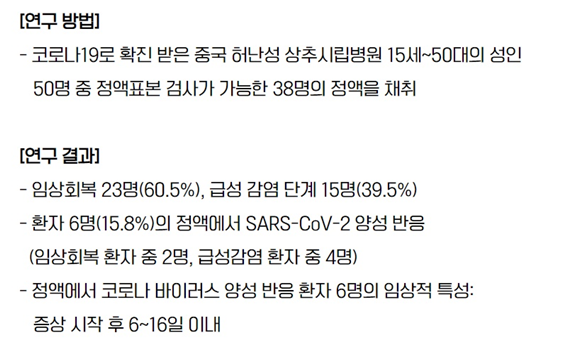
In May, JAMA Network Open posted a statement that read, "Coronavirus detected in semen." The results of the study were published. Until now, the main route of transmission of the virus was known to be droplet transmission through contact, but this time, the positive test result in semen has led many people to ask, "Could it be possible to transmit Corona through sexual intercourse?"I was afraid to do it.
Q. So, can I get the virus from sex?
It is not yet known whether the virus detected in semen is sexually transmitted. We cannot rule out the possibility that the virus debris may have been splashed through kissing prior to sexual activity.
A man's testicles, eyes, and placenta can act as 'immune privileged areas' and protect against severe inflammation. So, if the virus invades that area, there is a chance that the immune system will not be able to function properly and you will test positive for the virus.
This isn't the first time the virus has been detected in men's semen, and in the past, Ebola and Zika viruses have been present for months in the semen of men who have recovered. Since it has been shown that Ebola or Zika virus can be transmitted through sexual activity, the possibility of sexual transmission of COVID-19 cannot be ruled out.
As it is not yet known whether it is transmitted through sexual intercourse, additional studies are needed on the survival time of the virus in semen and the concentration of the virus in the semen. The researchers say there is no need to be "afraid" about the possibility of transmission through sexual intercourse.For safety, "abstaining from sex or using condoms may be considered as a means of preventing infection."
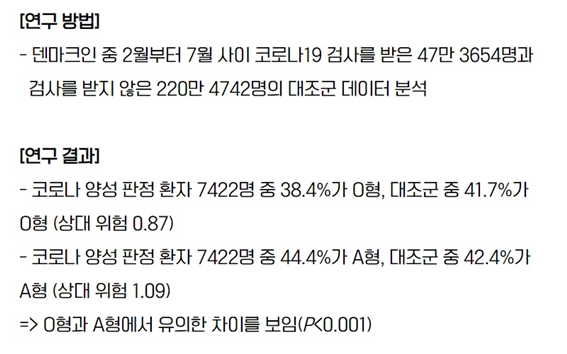
2. Are there any blood types that are more likely to get COVID-19?
At one point, on social media, it was said, "Type A is more likely to catch Corona, and Type O is less likely to catch Corona."It has become a hot topic as interesting research results have been published one after another to bolster the rumors that were thought to be ridiculous.
Studies have shown that people with blood type O are the most resusceptible to COVID-19 compared to other blood types, and are the least likely to develop severe illness if they do get infected, but is blood type actually linked to COVID-19 infection?
From the results of the study, it was concluded that type O is more resistant to COVID-19 infection than other blood types, with a significantly higher proportion of controls in type O, and there was no association between blood type and mortality after COVID-19 infection.
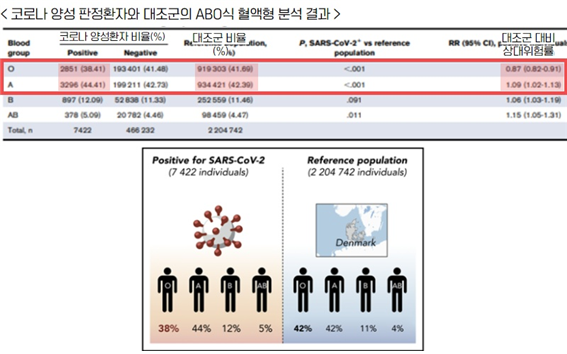
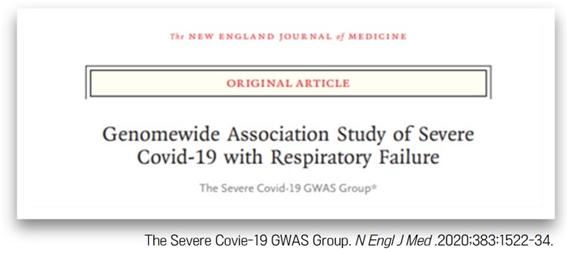
In addition, the world-renowned medical journal 'NEJM (New England Journal of Medicine)' has published a study that supports the above evidence.
The study included 1,610 patients with severe COVID-19 and 2,205 controls, and an age- and sex-adjusted meta-analysis found that people with type A blood were 45% more likely to develop severe COVID-19 than other blood types, while those with type O were 35% less likely to develop severe COVID-19 than other blood types.
That doesn't mean that type O is less likely to get infected than other blood types, not that you won't get it, so don't worry!
So, why is Type O so resistant to COVID-19?
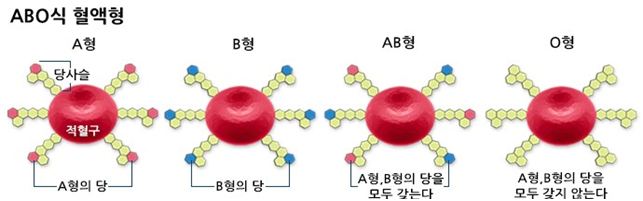
Blood type is expressed by antigens on the surface of red blood cells and antibodies in the blood, and it is said that type O may have fewer blood clotting factors than other blood types. Since one of the main causes of COVID-19 aggravation is blood clotting, it is also estimated that type O, which has relatively low clotting factors, is relatively less likely to develop severe COVID-19.
Previously, China, Russia, and Germany have also shown that type O has a lower infection rate and a lower chance of developing severe illness than other blood types, but many studies have shown similar results, so it is unlikely that there is any link with blood type. Once we find out what mechanism is related to blood type and COVID-19, whether blood clotting factors are really at the center of it, or whether the production of antibodies based on blood type affects the immune system when the virus invades, it can be applied to the development of COVID-19 treatments.
3. If you get COVID-19 after having a cold, are your symptoms mild?
Even if they are equally infected with COVID-19, some people are at risk to the point of being life-threatening, while others are asymptomatic and pass by without even knowing they are infected. Why this difference?
The common cold is one of the most common respiratory infections during the changing seasons.
Its symptoms are similar to the initial symptoms of COVID-19, such as cough, fever, chills, and muscle aches, which many people confuse the two.
However, the world's most prestigious journal Science reported that "the functions of the common cold and the COVID-19 virus are similar."The results of the study have been published and are attracting attention.
Coronavirus is one of the common cold viruses in humans, and the virus has mutated genetically to become COVID-19, and the researchers noted that the symptoms of COVID-19 are similar to those of the common cold.
The researchers found that the immune response of patients with a cold and those with COVID-19 was similar through T cells. When a virus invades, the body triggers an immune response, remembers the antigen, and later attacks the same antigen when the same antigen invades. The antigenic group of a cold virus antigen is similar to the spike of COVID-19, causing an immune response through T cells, and the property of antibodies that respond to similar epitopes of other antigenic substances is called cross-reactivity.
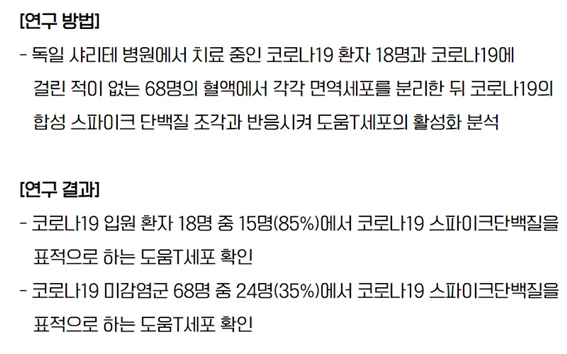
In addition, a study on immune T cells from the common cold and COVID-19 was published by a team of researchers in Germany, which was also published in the world-renowned journal Nature.
It was natural for patients with COVID-19 to have a T cell response to the COVID-19 spike protein because it is the same antigen, but even in the uninfected group, the T cell response occurred at a fairly high rate of 35%.Since the antigenic crystal sites of the cold virus and the COVID-19 virus are structurally similar, it can be interpreted that the antibodies produced when you have had a cold in the past have cross-reacted with the COVID-19 virus.
In other words, it can be assumed that the reason why the severity of symptoms varies from person to person even with COVID-19 infection is that the slight immune response caused by the cold coronavirus in the past has shown cross-reactivity to COVID-19.
Here are three interesting studies related to COVID-19.
COVID-19 has become a nationwide pandemic again. On the 13th, the number of new cases exceeded 1,000. If we don't get a firm grip on the current spread of COVID-19, our daily lives will continue to fall apart. Before developing vaccines and treatments, we need to practice social distancing and do everything we can to protect ourselves, such as washing our hands and wearing masks.
Many researchers around the world are still working to understand the clinical characteristics, route of infection, and mechanism of COVID-19. Understanding the key information about COVID-19 will spur the development of treatments beyond vaccines.
The FDA approved the Pfizer-BioNTech vaccine for emergency use on Jan. 11, and the COVID-19 vaccine rollout in the U.S. has begun today, with a total of 2.9 million doses on shipment across the U.S.
Of course, vaccination does not completely kill COVID-19.In the case of COVID-19, it mutates so quickly that it is unclear whether long-term immunity can be achieved through vaccination. Vaccine side effects cannot be overlooked either.
The best-case scenario would be for the virus to be completely contained, but if we have to coexist with COVID-19, I look forward to the day when we can be prevented by a COVID-19 vaccine, just like the flu that comes every year.





Comments (0)
There are no comments for this article. Be the first one to leave a message!